This made me reflect how medicine in the US is very instant, we want results and we want them now. Once the results come we want action to be taken immediately. It seems like there is always a test or image to follow up on and the care plan for patient's is dynamic changing moment by moment. Perhaps that is why I struggle when patients, families, nursing staff, administration and even attendings ask when something will be done or when the discharge will take place. I can give a rough estimate but in reality I'm not very accurate at predicting the future. That being said all I ask for is patience and understanding when I predict the wrong time, the wrong date or discharge a patient past 1 pm.
Moving on rounds this morning were incredibly brief. The woman with pancytopenia, fevers non responsive to antibiotics, and now crackles with associated hypoxia on room air is still ill. She refused to go to the bigger city, Hyderabad, for a second opinion on her bone marrow. The marrow read here was reactive but her clinical symptoms and lab studies seem to be consistent with a hematological (blood) malignancy. That leaves the Professor with a tough decision on calculating her next move. More to come on that tomorrow. The remainder of the 7 patients were seen quickly with new changes in management (except the dose decrease in the antibiotic).
After rounds the Professor took me to the Cardic Cath lab where her husband is a cardiologist. I was able to observe and interact with the cardiologist to see how evidence based medicine is modified under socioeconomical restraints. The hands of the physician's are tied when it comes to their degree of practice, they have the ability to perform what the guidelines say but if the patient can't afford the medication after the procedure the "gold standard" is obsolete. The case I observed was an elderly woman with three vessel disease and an EF of 20-25%. The CT surgeons AND the patient were not willing to accept the risks of bypass surgery. This left the cardiologist to at least perform a palliative stent to the RCA to help with her symptoms. The stents they use are bare metal stents. When a patient gets the procedure the government will pay for the procedure and one year of medications. After that the patient is on their own. Another fascinating aspect of the cath lab was when I walked into the back room to put on the lead jackets to avoid radiation exposure, there were woman on the floor with medical equipment spread on a blanket. There were syringes, catheters, guide wires, and instruments. Then the explanation followed...due to cost they have to reuse the medical supplies 4-5 times each. In the US the supplies are discarded after the procedure even if they weren't use. This is due to reducing the risk of infections. However here supplies are limited and valued. These woman spend their days cleaning and sterilizing the materials in order to give the patient's to opportunity to have a cath performed. The cardiologists use more femoral approaches than radial because the supplies for the femoral access can be reused 4-5 times instead of 2-3 like the radial supplies. Perhaps the risk of infection is the chance they have to take to survive. Who I am to judge. Although when I was in the OR, people were wearing open toe sandals, masks below their noses, the x-ray operator was on his cell phone, and the cardiologist "sterile" gown had a hole in the sleeve. I'm sure the infection control people from the US would have a heart attack had they seen this procedure suite.
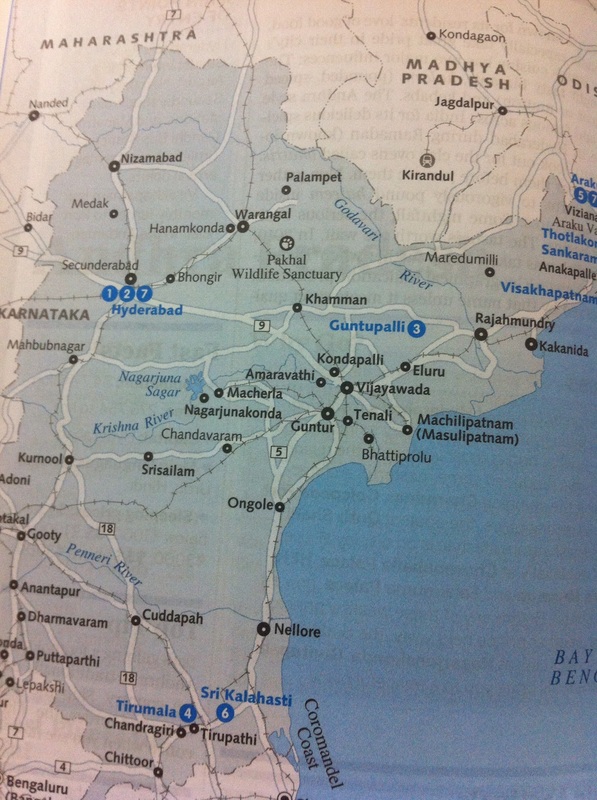
Map of Hyderabad
 RSS Feed
RSS Feed
